Reproduction – Chap 11 – Biology MDCAT
-
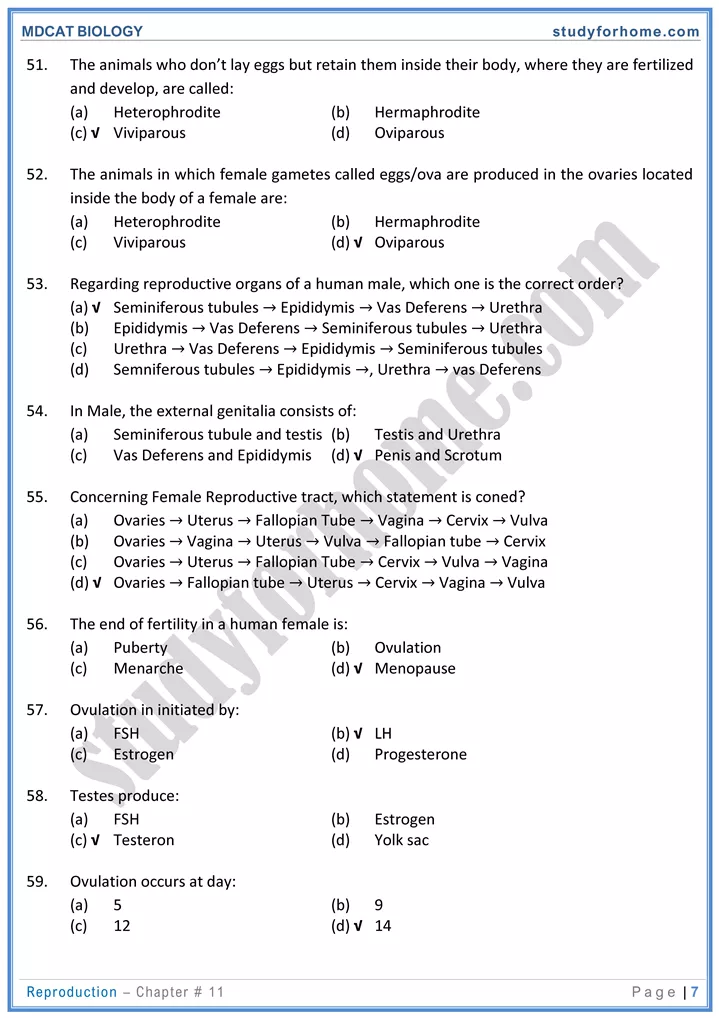
Male Reproductive System:
- The male reproductive system includes: gonads, accessory ducts, accessory glands and copulatory organ.
-
Gonads:
- The testes are male gonads which are situated outside the abdomen within a skin pouch, called scrotum.
- Each testis is divided into 250-300 lobules each lobule contains one to four tightly coiled and highly complex duct system called seminiferous tubules, in which cells of germinal epithelium divides to produce spermatogonia.
- Seminiferous tubules are the sites for spermatogenesis.
- Testes are also acts as endocrine glands because they produce male sex hormones, most important of which is testosterone.
- Seminiferous tubules also contain sertoli cells/nurse cells, which provide liquid medium, protection and nourishment to sperms while they are in the tubules. These cells also secrete inhibin hormone which serves to control the spermatogenesis at normal rate.
- Interstitial cells/leydig cells are present between the seminiferous tubules and secrete testosterone, essential for production of sperms and development of male secondary sexual characteristics during puberty.
- Both germinal epithelial cells and sertoli cells are under the control of FSH while interstitial cells are under the control of ICSH.
-
Accessory Ducts
- Once spermatozoa are produced, they move through the seminiferous tubules and enter a
- tubular network called the rete testis for further maturation.
- The spermatozoa are transported out of the testis by a series of efferent ductules.
- Epididymis is the proximal and highly convoluted portion of vas deferens. Its function is to transport and storage of sperms.
- Epididymis opens into another duct celled Vas deferens (sperm duct) and is the main duct of male reproductive tract.
- It joins with the duct of the seminal vesicles to form the short ejaculatory duct Here ejaculatory duct enters the prostate gland; then it empties into the urethra.
- In male, urethra is also called as urinogenital duct because it transfers both urine and semen outside the body.
-
Copulatory Organ:
- Penis is copulatory organ is used to transfer sperm into female reproductive tract.
- It consists mainly of tissues that can fill with blood to cause an erection.
-
Accessory Glands
- These are exocrine in nature and include seminal vesicles, prostate and bulbourethral/Cowper’s glands.
- A pair of seminal vesicles is located at the junction of sperm duct and ejaculatory duct.
- The prostate gland encircles the urethra just below the bladder.
- A pair of bulbourethral gland/Cowper’s gland is situated at the junction of ejaculatory duct and urethra.
-
Spermatogenesis:
- It is the process of sperm formation in males. This process takes place in the inner/germinal epithelium of seminiferous tubules.
- The spermatogonia divide by mitosis, forming a primary spermatocyte which undergoes meiosis-I, forming two smaller haploid daughter cells, called secondary spermatocytes.
- Each secondary spermatocyte after meiosis-Il produces two daughter cells, called spermatids. Each spermatid is a round, non-motile, and haploid cell.
- Spermiogenesis is a process in which spermatids change into motile and active sperms.
- During this process, a spermatid elongates, sheds its excess cytoplasm, and form a tail.
-
Female Reproductive System:
- The reproductive role of the female is far more complex than male. She not only has to produce gametes, but her body must be prepared to nurture a developing embryo for a period of a approximately nine months.
-
Gonads:
- Ovaries are female gonads which produce ova and release hormones.
- The paired ovaries flank the uterus on each side and each ovary is held in place within the peritoneal cavity by several ligaments.
- The ovaries are solid, ovoid structures. Within the ovary are many tiny sac-like structures called ovarian follicles each of which consists of an immature egg, called an oocyte.
- In adult women, one of the ripening follicles ejects its oocyte from the ovary in each month. This event is called ovulation.
-
Oviducts:
- The oviducts form the initial part of the female duct system. They receive the ovulated oocyte and are the site where fertilization generally occurs.
- It transfers developing in ovum from ova towards the uterus.
-
Uterus:
- The uterus or womb is a hollow, muscular organ, shaped somewhat like an inverted pear.
- The uterus has three portions: the fundus, the body and the cervix.
- The oviducts join the uterus just below the fundus and the opening of the cervix leads to the vaginal canal.
- Cervix is a narrow entrance to the uterus from the vagina. It is normally blocked by a plug of mucus.
- The wall of the uterus is composed of three layers;
-
Perimetrium:
- The perimetrium is the outermost thin covering layer of the uterus.
-
Myometrium:
- The myometrium is the middle thick muscular layer composed of bundles of smooth muscle, which contracts rhythmically during childbirth to expel the baby from the mother’s body.
-
Endometrium:
- The endometrium is the inner spongy lining of the uterine cavity. If fertilization occurs, the young embryo is implanted into the endometrium and resides there for the rest of its development. The main functions of uterus are to receive retain and nourish a fertilized ovum.
-
Vagina:
- The vagina (opening is called vulva) is a thin-walled long tube and extends from the cervix to the body exterior.
- Vagina is often called the birth canal as it provides a passageway for delivery of an infant and for menstrual flow. The urethra is embedded in its anterior wall.
-
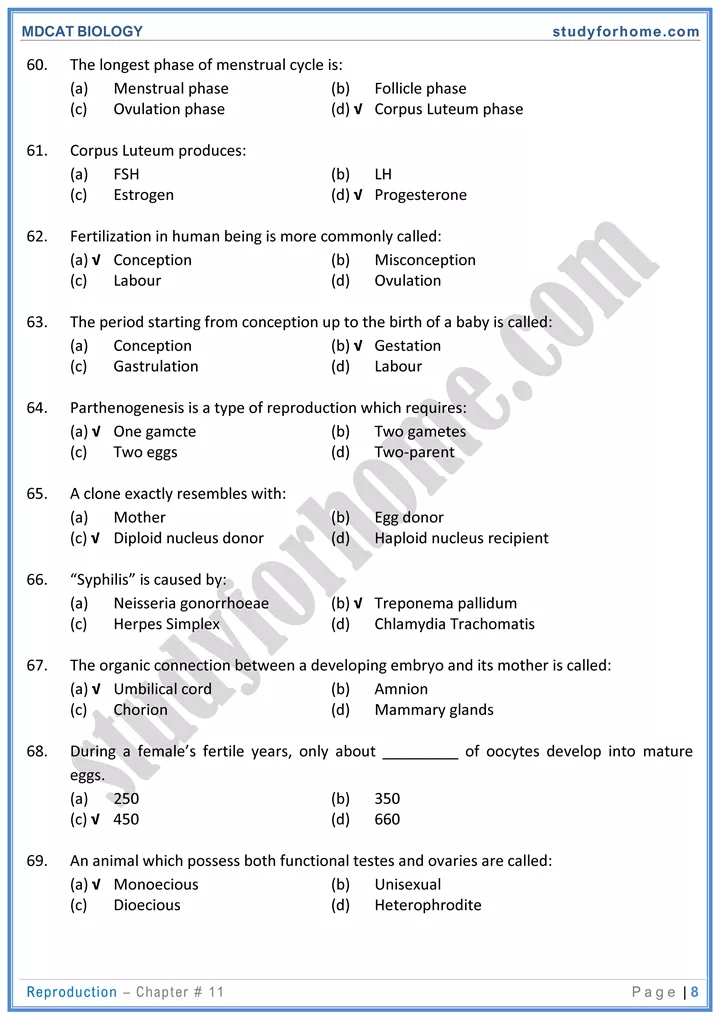
Oogenesis:
- Gametogenesis in the female is known as oogenesis and result in the formation of ova/egg.
- Oogenesis starts before birth when oogonia divide mitotically to produce primary oocytes.
- These primary oocytes are enclosed in groups of follicle cells.
- Primary oocytes undergo meiosis-I but are arrested at prophase-I.
- At puberty, primary oocyte completes meiosis-I and gives rise to haploid secondary oocyte along with 1st polar body.
- Secondary oocyte undergoes meiosis-II but arrested in metaphase-II. It is released in this stage from ovary and does not proceed further until fertilization.
- If fertilization occurs, then secondary oocyte divides to form ovum and 2nd polar body.
- In human female only one ovum is usually discharged from the ovary at one time, this phenomenon is called ovulation.
-
Menstrual cycle:
- In female, production of egg is a cyclic activity as compared to male.
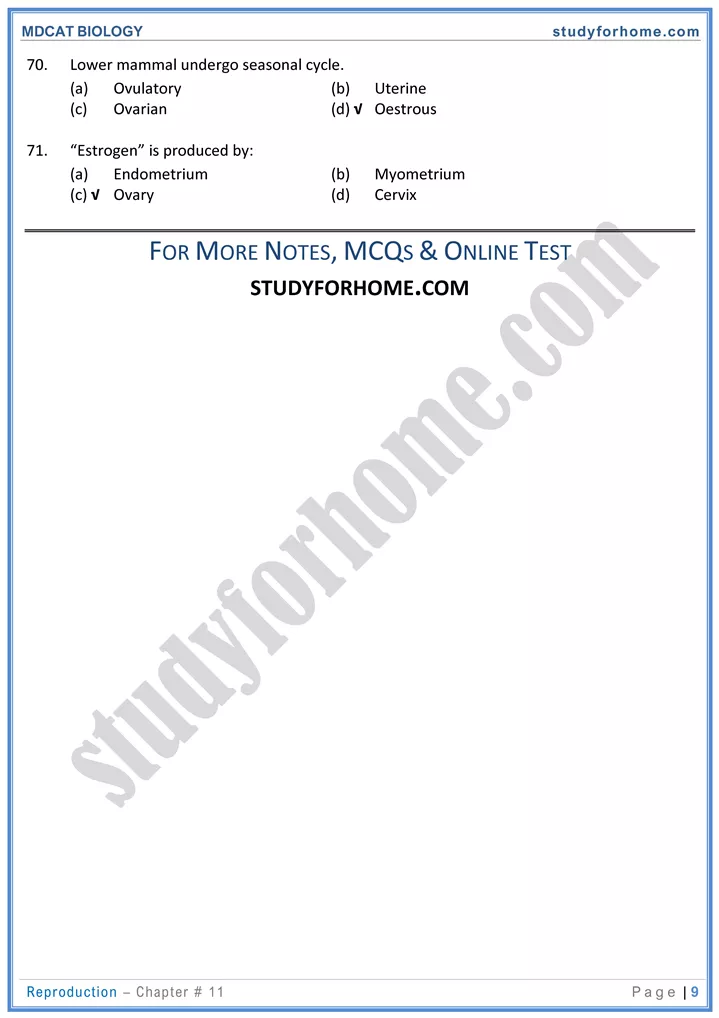
- Oestrous cycle is reproductive cycle in all mammalian female except humans. In human female, it is called menstrual cycle.
- Menstrual cycle involves changes in the structure and function of the whole reproductive system.
- ovulation and menstruation occur at puberty. Start of menstrual cycle is called menarche. Its complete stop or end is called menopause. This cycle is completed in approximately 28 days (average of 21-35 days).
- The events of the menstrual cycle involve the ovaries (ovarian cycle) and the uterus (uterine cycle). Events of menstrual cycle are regulated by pituitary gonadotropins.
- Based upon changes and hormonal regulation, the cycle can be divided into three phases i.e., menstrual phase, proliferative phase and secretory phase.
-
Menstrual Phase (Days 1—5)
- In this phase, the uterus sheds all but the deepest part of its endometrium.
- The thick, hormone-dependent functional layer of the endometrium detaches from the uterine wall, a process that is accompanied by bleeding for 3—5 days.
- The detached tissue and blood pass out through the vagina as the menstrual flow.
- At the beginning of this stage, ovarian hormones are at their lowest normal levels and gonadotropins are beginning to rise. Then FSH level be ins to rise.
-
Proliferative/Pre-Ovulatory Phase (Days 6—14):
- Follicle stimulating hormone (FSH) during the first days of the cycle stimulates few ovarian follicles.
- Only one follicle develops. Rest stop to grow and finally disintegrate (follicle atresia), while one dominant follicle in the ovary continue to mature and becomes mature follicle (Graffian or vesicular follicle), in which oogenesis occurs.
- FSH also stimulates the graffian follicle to secrete estrogen which in turn governs the vascularization of endometrial lining of uterine wall.
- Estrogen has negative feedback upon FSH, therefore, as the concentration of estrogen rises the level of FSH falls. This is a signal for anterior pituitary to release LH.
- At the end of the proliferative stage (day 14) LH causes ovulation which takes less than five minutes.
- LH also converts the ruptured follicle to a yellowish glandular mass called corpus luteum.
-
Secretory/Post-Ovulatory Phase (Days 15—28)
- During the secretory phase, the endometrium prepares for implantation of an embryo.
- Rising levels of progesterone from the corpus luteum act on the endometrium, causing the arteries to extend and converting the functional layer to a glandular secretory layer.
- uterine glands enlarge, coil and begin secreting nutritious glycogen into the uterine cavity.
- If fertilization has not occurred, the corpus luteum begins to degenerate towards the end of the secretory phase as LH blood levels decline.
- Progesterone levels tall, depriving the endometrium of hormonal support and endometrial cells die, setting the stage for menstruation to be in on 28th